Department of Radiology
Lung cancer is a very serious health concern caused in large part, but not entirely, by smoking. Francine L. Jacobson, MD, MPH, of Brigham and Women’s Hospital, advises patients to stop smoking to decrease their risk of developing lung cancer. Even if you’ve stopped smoking, you may be at increased risk of developing lung cancer. If you’re 50 to 80 years old, the risk is high enough to warrant screening every year. Dr. Jacobson notes that one life is saved for every 320 lung cancer screenings.
Email: bwhlcs@partners.org
Phone: 617-525-3515
Scheduling: 617-983-7020
Fax: 617-983-7122
Medical Director of the Lung Cancer Screening Program: Suzanne C. Byrne, MD
When it comes to lung cancer, the earlier the detection, the better the prognosis. Studies have shown that patients at increased risk who were screened with low dose CT (LDCT) rather than a chest X-ray, had 20 percent fewer deaths from lung cancer. Brigham and Women's Hospital/Brigham and Women's Faulkner Hospital Imaging screens high-risk patients for lung cancer screening at multiple locations using low-dose CT.
"The best way to prevent lung cancer is to stop smoking, but you don’t have to stop smoking to be screened." - Francine Jacobson MD, MPH
The screening CT scan is a very quick and painless procedure. It usually takes 15 minutes or less to complete and requires no needle stick or special preparation. It’s best to wear loose, comfortable clothes with no metal like zippers or underwire bras. You may eat before and after the exam.
The test itself is performed in less than a minute. You will be asked to hold your breath briefly.
What happens during a lung screening exam?
Learn more about lung cancer screenings.
Lung cancer forms in tissues of the lung, usually in the cells lining air passages. It starts from a single cell, but usually includes millions of cells by the time it can be seen by an X-ray. Cancer cells lose their previous function in the body. Instead they grow faster than regular cells. They cause the body to weaken and prevent organs from working. The two main types of lung cancer are small cell lung cancer, which spreads quickly, and non-small cell lung cancer, which is more common and spreads slowly. More than 238,000 Americans are diagnosed with lung cancer each year. Treatment depends on the type and stage of lung cancer and may include one or more treatments, including surgery, chemotherapy, radiation therapy or targeted drug therapy.
There are two major types of lung cancer:
Smoking tobacco is the most significant risk for developing this type of cancer, typically affecting people older than 45. Factors that contribute to an increased risk for developing lung cancer include:
Lung cancer may not cause any symptoms and may be found on a routine chest X-ray or low-dose chest CT scan. Signs and symptoms of lung cancer may include:
Diagnosis of lung cancer often includes a number of different tests and procedures, many conducted by your thoracic surgeon:
MRI, PET or bone scans determine if the cancer has spread from where it started into other areas of the body. Diagnosis of lung cancer often includes a number of different tests and procedures, many conducted by your thoracic surgeon:
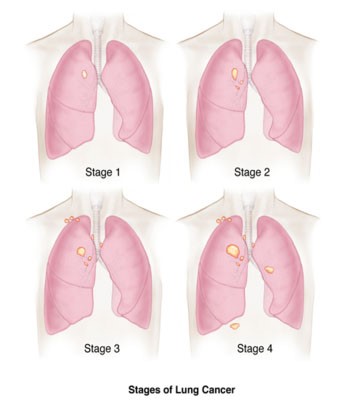
The process used to find out if cancer has spread within the lungs or to other parts of the body is called staging. The stage is determined from the results of physical exams, imaging tests and biopsies that have been done. The process used to find out if cancer has spread within the lungs or to other parts of the body is called staging. The stage is determined from the results of physical exams, imaging tests and biopsies that have been done.
Depending on its type and stage, lung cancer may be treated with surgery, chemotherapy radiation therapy, local ablation including laser therapy or a combination of treatments. Treatment options include:
Surgery is usually the best option for treating early-stage lung cancer and may be used to remove a portion of the lung or the entire lung. Our thoracic surgeons have pioneered the use of minimally invasive video-assisted thoracic surgery (VATS), and continue to develop innovative approaches to achieving the best outcomes for lung cancer patients.
Types of Surgery
Minimally Invasive Surgery
Using minimally invasive surgery techniques over traditional surgeries offers patients many benefits: improved accuracy and visualization, minimized trauma to tissue, less bleeding, decreased pain, less scarring and a shortened recovery.
Radiation therapy uses high-energy rays to kill or shrink cancer cells. Radiation is often used in conjunction with chemotherapy before surgery to shrink the tumor. Brigham and Women’s Faulkner Hospital’s Department of Radiology uses the most advanced equipment and techniques to deliver radiation to cancerous areas, while avoiding exposure to normal tissues. More importantly, radiation experts work closely with your surgeon to create a specialized treatment plan just for you.
Please call the Brigham Lung Center at 617-278-0810 for further information or visit the Brigham Lung Center website (opens on the Brigham and Women's website).
The U.S. Preventive Services Task Force (USPSTF) has revised the recommended ages and pack-years for lung cancer screening. They now recommend that adults aged 50 to 80 years who have a 20 pack-year smoking history and currently smoke or have quit within the past 15 years:**
**Check with your insurance company to see if you are covered for screening.
Speak to your primary care physician to see if you qualify for LCS CT. All patients require a physician order.
The LCS scan reduces the radiation dose to the patient by only scanning the area of the lungs. A normal chest CT scan uses a higher dose to see additional structures such as the heart and mediastinum, which are more difficult to see using low dose techniques. The dose used in a LCS CT is similar to that seen in screening mammograms.
Call the number on the back of your health insurance card and ask a representative about your coverage.
You should be in your best usual state of health. This may include a long-standing cough or shortness of breath due to smoking. The test should not be performed when you have new symptoms, such as fever, chest pain, a new or changing cough, shortness of breath that you have never felt before, coughing up blood, or unexplained weight loss.
Radiation can increase a person’s risk of cancer 20 or more years later. No test, including lung cancer screening CT, is perfect. Important medical conditions, including lung cancer may go undetected. Twenty five to 30 percent of the time, findings may require additional imaging or evaluation. Small lung nodules are very common, and more than 97 percent are not cancer although they can cause anxiety. Repeating the examination in 3 months is the most frequent follow-up exam to track nodules. Occasionally, patients need a procedure such as a biopsy that will only be performed with your informed consent.
Areas of your body next to your lungs are partially imaged. In a small percentage of cases (5 to 10 percent), the CT scan will show an abnormal finding in one of these areas, such as your kidneys, adrenal glands, liver or thyroid. Your healthcare provider who ordered your exam can help determine what, if any, additional testing you may need.
Your healthcare provider who ordered your exam will receive a copy of your results. You can sign up for Patient Gateway to view the results directly.
Brigham and Women's Hospital/Brigham and Women's Faulkner Hospital’s Lung Cancer Screening program is approved by the Massachusetts Department of Public Health Radiation Control Program as a “healing arts screening program.” Additionally, the American College of Radiology recognizes our site as a “designated Lung Cancer Screening Center.” These designations assure our patients that they will receive the very best quality care while minimizing the radiation dose.
Offering comprehensive medical, surgical and psychiatric care as well as complete emergency, ambulatory and diagnostic services to residents of southwest Boston and the surrounding suburbs.
Learn more about BWFH